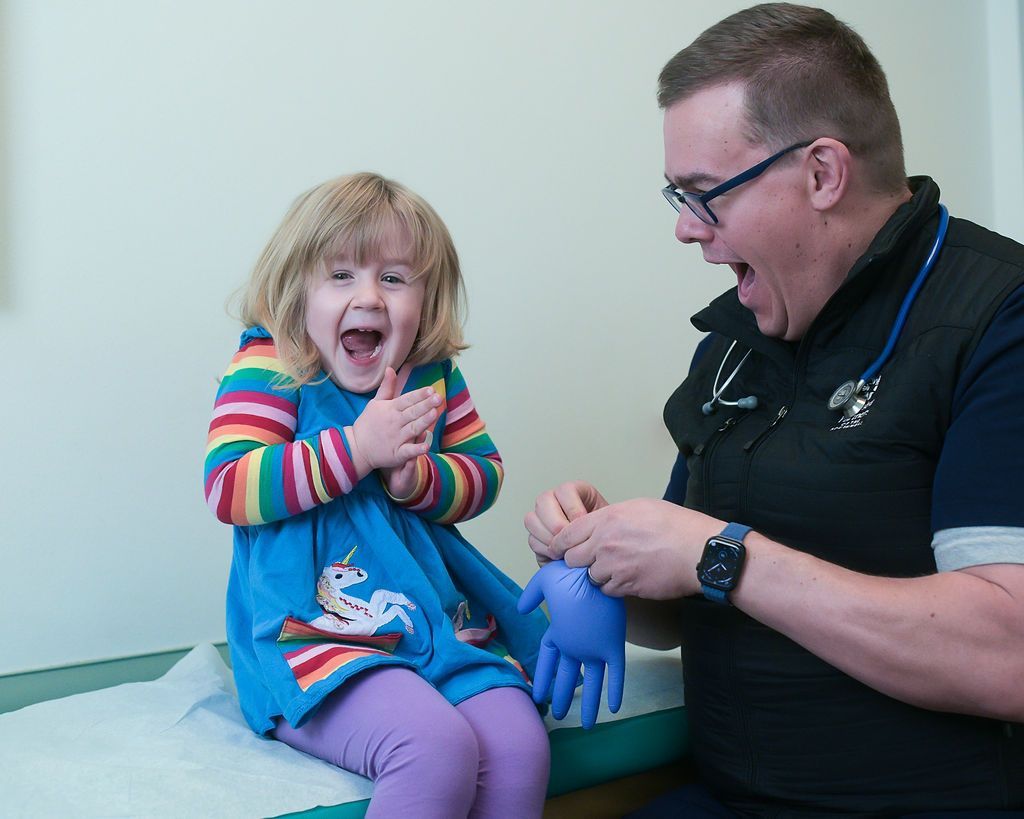
Wonderful experience such great Dr. I will be making it my new pediatric office for my children for sure. They were so pleasant and took there time and and u felt like your children were in the very best hands. Thank u
Cory R
Every time I take my children here, I'm so grateful for the care provided. That's why I choose to drive over an hour to have my children seen by them; it's worth it. Every doctor that has seen my children here (including a severely special needs child), has been knowledgeable, compassionate, actually listens and values the parents input, and just genuinely 'cares.' As a patient's parent who has been taking their children to Pediatric Partners for 12 years, I wouldn't change a thing about the amazing care my children have received. Thank you guys ♡!!!
Krista M
We waited less than 1 minute. Our nurse was there immediately and very friendly. Taylor was our provider and she was amazing! She spent a ton of time with my daughter addressing every concern and we came up with a very good plan. Very impressed and very pleased with the service we were given.
Gabe G
We love Pediatric Partners. Taylor Hayes is an amazing provider. She is very competent and considerate. I feel very comfortable taking my child there.
Krista H
We’ve taken both our daughters here since their births and have always received excellent care from the techs to the doctors. We live an hour away from the Durango office, but the care is worth the drive for us.
mattabe86
We have always been pleased with the care and professionalism we receive from PPoftheSW. Every physician and nurse we have seen for the past 14 years has been attentive, compassionate and supportive. We have recently been very pleased with Amanda Stanton, DO and Savannah Porter, PA-C. They are amazing fits for our kids and truly try to treat them with individualized care, not a “one size fits all” mentality. They have holistic approaches to care that goes beyond just their physical health, but takes care of their mental health, as well. We always feel like we have a team helping us work through any concerns within the standards of medicine and health that we feel comfortable with for our family, even when it requires a little “out of the box” solutions.
Natalie T
We've been going to this office for 17 years. They always get us in quickly, a key benefit with sick kiddos. And they've helped us navigate numerous illnesses and conditions. Many years of good advice!
Angie
Ryan Conrad is the best! Very knowledgeable, thorough and my kids love him!
Jessie S
Dr. Marsh (and the whole PPSW team) are great. We come up from Farmington to get seen and couldn’t be happier. Everyone is friendly, rooms are clean/comfortable, and the providers really seem to care and are clinically sound. Parking can be difficult but that’s not the fault of the clinic.
Christopher C
We couldn’t be more thankful for everyone at pediatric partners. No matter how big or small our problem, we have been treated with the upmost care, compassion and professionalism. A special shout out to P.A. Ryan for making sure all my questions are answered especially working on a limited time schedule. His responses are thoughtful, informative and actionable! A past due thank you to Dr. Marsh for working with us diligently towards getting our baby off oxygen using the most up to date and science backed approach. I feel safe in your care and as a nervous mama that goes a long way.
Heather C